Chemsex: the dangerous combination of sex and amphetamines
The phenomenon first appeared in the United States and certain large European cities in the early 2000s. "Chemsex," or chemical sex, combines sexual intercourse with the use of drugs such as cocaine, ketamine, or cathinones in a novel way. It is now growing in France, while remaining largely unknown—especially in terms of its short- and long-term dangers.
Edouard TUAILLON, University of Montpellier

A synthetic product derived from a substance found in khat leaves, cathinones are enjoying growing popularity. Part of the large amphetamine family, they owe their popularity to the fact that they increase the release of dopamine, a key neurotransmitter in the reward circuit.
These synthetic molecules have only recently arrived in France: the first seizure dates back to 2007. Since then, their use, long restricted to a small circle of experimenters frequenting specialized blogs (e-psychonauts) or former drug addicts, has quickly grown among MSM (men who have sex with men).
This success is partly due to the characteristics of the drug itself, but also to the simultaneous emergence of several factors that have contributed to its popularity: mobile dating apps, GHB (which we will discuss later), and the effectiveness of drugs designed to prevent and treat human immunodeficiency virus (HIV).
The many factors behind its success
First, it should be noted that synthetic cathinones are relatively inexpensive due to their relatively simple production process, even though their effects are powerful and tolerance does not develop with regular use. This is a notable difference from ecstasy, which requires users to space out doses in order to maintain maximum effect.
We should also highlightthe impact of geolocation-based mobile dating apps on behavior, the most famous of which (Grindr) was launched in 2009. These apps make it easier to meet partners who share the same sexual desires, but their spread has been accompanied by the closure of gay social venues. Paradoxically, the ease of meeting people has sometimes been accompanied by painful emotional isolation among people who nevertheless have numerous sexual partners.
Then, after decades marked by fear of AIDS, improved treatment made a new period of sexual liberation possible in the 2000s. Although antiretroviral treatments still cannot cure the disease, they are very safe, well tolerated, and prevent HIV transmission. In addition, pre-exposure prophylaxis (PrEP), authorized in France since July 2017, effectively protects people who have unprotected sex with multiple partners from HIV.
Finally, GHB (4-hydroxybutanoic acid or γ-hydroxybutyrate), another synthetic drug that became popular in the early 2010s, contributed to the success of chemsex. This neurotransmitter is naturally synthesized by certain neurons and binds to GHB and GABA (γ-aminobutyric acid) receptors in the brain, as do alcohol and anxiolytics. Its relaxing and sedative effects explain its medical use as an anesthetic.
Classified as a narcotic since 1999, GHB is theoretically difficult to obtain... but this is far from the case with GBL (gamma-butyrolactone). A solvent widely used in industry, GBL is rapidly metabolized into GBH after ingestion. Commonly referred to as the "date rape drug" because it is sometimes used as a chemical sedative, many users deliberately combine it with cathinones in chemsex practices.
Powerless, the medical world has watched the combined use of cathinones and GBL/GHB emerge over the past 10 years through the prism of the treatment of sexually transmitted infections.
Related to sexually transmitted infections
At the turn of the 2010s, issues related to drug use appeared to be secondary in the hospital care of people living with HIV. Most former drug users were either in withdrawal or undergoing substitution treatment with Subutex or methadone; psychotropic drug use involved the same products as in the general population, namely tobacco, alcohol, benzodiazepines, and cannabis.
However, it was noticed that a small number of patients surprisingly had multiple sexually transmitted infections: HIV, hepatitis A and C, but also syphilis, gonorrhea, chlamydia, etc. In 2013, the consultation service at Montpellier University Hospital, where I am one of the practitioners, reported cases of multiple sexually transmitted infections (STIs) linked to the use of cathinones. These patients exhibited particularly risky sexual behavior, which appeared to be encouraged by the use of drugs that were little known at the time.
A survey conducted in the same year among 1,000 HIV-infected patients in the consultation service revealed that 2.7% of them used cathinones and 7.1% used GBL.
Commonplace use
Since then, consumption has become considerably more commonplace. Starting in 2017 with the arrival of PrEP, many hospital consultations have incorporated a preventive component for people at risk of HIV infection. Whether they are young people (starting their sexual lives in a less anxiety-provoking era) or older people (enthusiastically embracing their return to single life after a period in a relationship), the freedom provided by this prevention and dating apps also exposes the most vulnerable to the alienation of chemsex.
New terms have crept into routine consultations: "chem" for chemsex, "3-MMC" or "4-MEC" for 3-Methylmethcathinone and 4-Methylethcathinone (mephedrone), "G hole" for loss of consciousness due to GBL/GHB overdose, etc.
The consumer profile has been enriched with multiple faces driven by just as many motivations: shy thirty-somethings looking to let go, fifty-somethings seeking a renewed libido, homosexuals struggling with a homophobic upbringing or culture, or simply hedonists.

SElefant/Wikimedia/Pfizer, CC BY-SA
At the same time, it should be noted that requests for prescriptions for erectile dysfunction medication have become more frequent at the end of consultations for the prevention or treatment of sexually transmitted infections: cathinones stimulate libido... but inhibit erection. As a result, regular users of these synthetic products are often already consuming high doses of Viagra-type drugs in their early 20s or 30s.
The problem of craving
The many new users we are now seeing in consultation are unaware of these risks, such as addiction. However, once chemsex involving cathinones becomes a regular practice, it is rare for users to stop. The craving, or impulsive need to use, is very pronounced with this amphetamine: 85% of users may experience it. The risk of addiction is estimated at 30%.
Craving is one of the main problems associated with cathinone use and is explained by the activation of the reward circuit. The urge to use comes from the persistence of high dopamine levels, while serotonin levels (another neurotransmitter that normally counterbalances the effect of dopamine) have returned to normal, causing a period of stimulation and, secondarily, a compelling need for the drug.
In rodents, where craving has been confirmed by cathinone self-administration experiments, it has been observed that, compared to other drugs such as methamphetamine, rats administer very high cumulative amounts on a daily basis (31.3 mg/kg/day for cathinone versus 4 mg/kg/day for methamphetamine). Among the drugs currently in use, the risk of abuse associated with synthetic cathinones is therefore one of the highest observed.
On the slope of addiction
Over the past four years, tragic stories linked to cathinones have become commonplace in hospitals and STI information and testing centers. The most vulnerable individuals are the most likely to see their consumption increase, their social integration fragment, and their mental health shift toward depression or paranoia.
The recent nature of cathinone use in combination with GBL, as well as the relative rarity of complete withdrawal among regular users, suggests that health problems associated with prolonged use are likely to increase in the medium term. What will become of this generation, which is experimenting with new practices combining PrEP, mobile dating apps, and synthetic drugs, in ten years' time?
The descent into addiction often involves a series of stages. The method of consumption is one such stage. Cathinones can be consumed orally or even rectally. However, these digestive routes, associated with a slow increase in blood concentrations of cathinones, are abandoned by the majority of experienced users in favor of the nasal route, which allows for a rapid increase in blood levels. Finally, there is the injectable route, which provides an even more intense effect (known as " slam" in English).
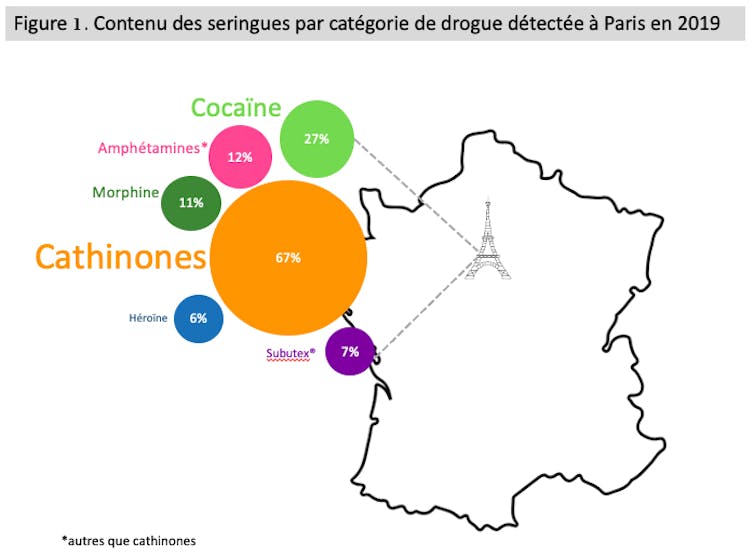
E. Tuaillon/Based on European Monitoring Center for Drugs and Drug Addiction (2021), An analysis of drugs in used syringes from sentinel European cities: Results from the ESCAPE project, Provided by the author
This latter practice marks a symbolic and pharmacological transition to drug addiction, leading some users to compulsive injections several times a day. The frequency and context of use are further steps on the path to cathinone addiction.
From festive events to everyday practice
Fortunately, there are still many occasional users who limit their chemsex to a few festive occasions throughout the year. However, others use it regularly, particularly at weekends.
In this case, consumption often begins on Friday evening and can continue through Saturday and sometimes into Sunday. It often becomes a regular occurrence, like a festive weekend ritual, disrupting mood and work during the week when the brain is starved of dopamine.
Many new regular chemsex users have linkedtheir increased use of cathinones to the health restrictions imposed by the COVID-19 pandemic.
The sexual context of product use is another indicator of the severity of addiction. For people with little or no dependence, sexual activity remains possible and desirable without cathinones. For others, sexuality is only attractive in the context of chemsex. At the next stage, the very notion of chemsex fades away in favor of drug use alone.
In the most severe cases of addiction, the product is consumed two to three times a week, often by injection, and several times in the same day. It causes periods of wakefulness lasting 48 to 72 hours, followed by periods of prolonged sleep.
As with other drugs, the risks associated with cathinones and GHB consumption stem from the inexperience of new users and the consequences of addiction among experienced users, including accidental deaths at home or on public roads, suicide, and cardiorespiratory arrest due to overdose.
The number of deaths directly or indirectly attributable to these products is difficult to determine due to the difficulty in distinguishing between accidents and suicides linked to their use. In 2017, around 20 deaths likely linked to chemsex were reported by the Regional Coordination Committee for the Fight against HIV in Lyon (COREVIH Lyon-Vallée du Rhône).
Prevention: a real priority
Many chemsex practitioners do not consider themselves drug users. Those who are aware of their addiction often refuse treatment that is difficult and does not offer substitution therapy.
Prevention must therefore become a priority. We need to explain the neurological mechanisms of addiction and encourage regular, occasional, and potential users to stop denying the problem and recognize the difficulties faced by those around them who have become addicted.
Awareness helps prevent or reduce the risks associated with the use of cathinones and GBL.
Beyond specialized hospital consultations, society as a whole needs to become aware of the problem of cathinones.
For now, chemsex is being discussed in the press, on radio shows, and in literature. But this is happening without any prevention measures from public authorities, while at the same time, repression is being put in place.
For a long time, sellers, who were themselves consumers and socially well-integrated, were rarely bothered by the police and the justice system. This is no longer the case. Consumers are being summoned to court for reminders of the law, and prison sentences are being handed down to sellers. In early 2021, a doctor from the Montpellier region, who was both a consumer and a supplier, was convicted and banned from practicing medicine.
In this context, the absence of a ban on the sale of solvents containing GBL is paradoxical. In 2011, France enacted a decree prohibiting its sale to the public, but not its sale to professionals.

United States Department of Justice/DEA/Wikimedia
GBL therefore remains available, and its consumption has increased in recent years. The French National Agency for Medicines and Health Products Safety (ANSM) raised the alarm in December 2018. The ANSM's recommendations, which aimed to tighten restrictions on the sale of GBL, appear to have fallen on deaf ears for the time being.
While prevention campaigns should be a priority, they remain very rare. One example is the campaign launched in 2018 by COREVIH Lyon-Vallée du Rhône, which includes a website, conferences, and videos. It should also be noted that in March 2021, the Paris Council voted in favor of a "chemsex information and risk reduction plan" and hopes to have tools in place by the end of February 2022. One of the project's leaders, Paris Deputy Mayor and activist Jean-Luc Romero-Michel, lost his husband in 2018 to an overdose.
It is to be hoped that these initiatives mark the beginning of a new era, one in which public authorities respond to the challenges of preventing the risks associated with synthetic amphetamines.![]()
Edouard TUAILLON, University Professor and Hospital Practitioner. Areas of expertise: infectious diseases, virology, sexual health, University of Montpellier
This article is republished from The Conversation under a Creative Commons license. Readthe original article.