Dietary supplements, meditation, osteopathy: how effective can alternative medicine be?
Today, alternative medicine is in great demand. A diet here. A dietary supplement here. Herbal teas, tai chi, hypnosis methods, psychotherapies, manual therapies, video games, connected health objects, ergonomic pillows...
Gregory Ninot, University of Montpellier
The list of products and methods available to treat conditions outside conventional treatment seems endless. Alternative medicines are now available in hospitals, GP surgeries and specialist practices. More than 100 million people use them in Europe, according to a survey conducted by the CAMBrella European program in 2012.
These solutions to our health problems are most often presented as effective and safe. But not all of them are created equal. All over the world, researchers are assessing their health benefits and risks. With, already, solid results.
To make this knowledge more accessible, our team from the universities of Montpellier launched in February the very first search engine dedicated to these "non-medication interventions" (NMIs), called Motrial. A sort of "Google of alternative medicine studies". Designed for researchers, it can also be used by doctors to find out what to suggest, for example, to a patient with back pain.
Complementary or alternative medicine?
The demand for rigorous evaluation of alternative therapies has become increasingly pressing over the years. In 2011, the French National Authority for Health (HAS) called for the "development of the prescription of validated non-drug therapies". In 2013, the French Academy of Medicine called for more appropriate use of "complementary therapies".
Citizens are also concerned, as shown by the survey published in 2014 by Eurocam, a foundation for complementary and alternative medicine.
For the questions that arise are many: what are the real benefits of these interventions? What risks do they entail for their users? Are they complements or alternatives to conventional treatments? Do they open the door to abuses such as financial scams, psychological control leading the person to refuse conventional care, or recruitment by cults? Do they have to be prescribed by a doctor?
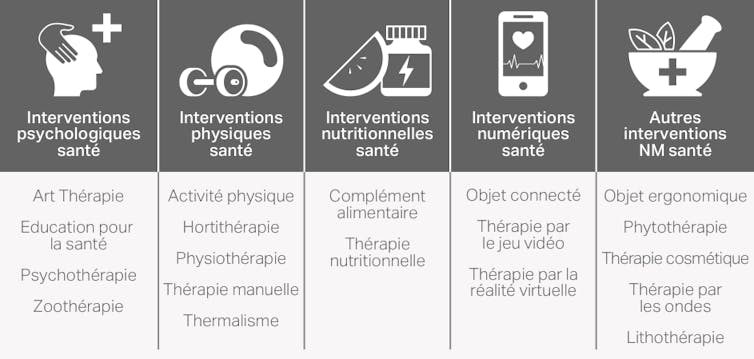
CEPS Platform Montpellier Universities
An effective osteopathic program for back pain
Because it would be simpler for everyone, we'd like science to be able to make a global and definitive decision on the effectiveness of each discipline. Osteopathy, for example. This technique of manipulating joints and muscles is now well known. So, we ask ourselves, does it work, or doesn't it?
There is no serious answer to such a question. We can, however, attest to the positive effects of a specific osteopathic method for a given disorder - in other words, a "non-drug intervention". For example, a British study of two months of osteopathic treatment for low-back pain showed a reduction in the intensity of pain.
Similarly, instead of talking about "dietary supplements" in general, we need to look at a particular product, with a certain dosage over a certain period of time, in relation to a specific health problem. A team of Iranian researchers, for example, studied aloe vera gel. They observed that a 300 mg capsule every two hours for two months in diabetics (type 2) improved their blood sugar levels - but not their blood fat (lipid) levels.
Evidence-based alternative medicine
Today, we are witnessing the advent of evidence-based medicine, with practices underpinned by science. This trend encourages us to move away from the nebulous concept of "alternative medicine". Non-drug interventions (NDIs) are to be studied with the same rigor as drugs. Eventually, each NMI will come with a globally recognized name, a description of its content, objectives based on health indicators, a target population, an explanatory theory, qualified professionals ready to implement it, and scientific publications validating it.
Researchers evaluating these interventions are already using clinical trials - just as they would for future cancer chemotherapy. A clinical trial is an experimental study that compares the health benefits and risks of a solution in one group of people with one or more other groups known as controls, or placebos. Clinical trials break with the magical thinking, fads and marketing hype that all too often accompany alternative medicine.
The number of such trials in NMIs has been rising steadily since the turn of the century. Every year, over 50,000 new publications concern non-drug clinical trials. Their methodological quality is also improving, thanks in particular to the initiatives of groups of researchers. In France, the Collège universitaire interdisciplinaire de médecine intégrative et thérapies complémentaires (CUMIC) was created for this purpose in 2018, coordinated by two medical professors Julien Nizard and Jacques Kopferschmitt.
A meta-analysis on physical activity and breast cancer
Another tool for evaluating NMIs is meta-analysis. This is a systematic review of the scientific literature, combined with statistical techniques. By combining data from all relevant studies, these meta-analyses provide more reliable estimates of the effects of a treatment or prevention strategy than those derived from a single study. Health authorities, national agencies and learned societies rely heavily on these meta-syntheses to issue their recommendations.
For example, the meta-analysis published in 2013 by our laboratory, Epsylon, focused on the dose of physical activity useful for reducing fatigue during breast cancer treatment. This work shows a reduction in the fatigue felt by women, if their physical activity practice is less than 2 hours per week. This meta-analysis is based on 17 studies involving a total of 1,380 patients.
Still in breast cancer, another example concerns psychotherapy. A meta-analysis published in 2017 by a German team looked at mindfulness meditation, practiced as an adjunct to biological tumor treatments. This is the method of the American John Kabat-Zinn, an 8-week program designed to reduce stress(Mindfulness Based Stress Reduction or MBSR). Conclusion: compared to standard care alone, this program brings additional benefits by acting on anxiety and depression. This meta-analysis was based on 10 studies involving a total of 1,709 patients.
Behavioral therapy more effective against depression than light therapy
This tool can also be used to compare NMIs. For example, the meta-analysis by a Dutch team published in 2017 gathered 11 studies (including 1041 patients) on different ways of treating depression in general practice. Between cognitive behavioral therapy (CBT), a physical activity program, problem-solving psychotherapy, a behavioral change program and light therapy, the authors conclude that CBT seems to be preferable - while encouraging further studies to confirm this finding.
This meta-analysis work, however, is particularly time-consuming and difficult when it comes to NMIs. That's why we launched the Motrial meta-search engine, with the aim of saving researchers time.
Motrial sorts and organizes scientific publications by identifying the main publication, the ethics committee declaration number, the protocol registration number with the competent authorities, the funding sources, the name of the sponsor and the country in which each study was carried out. It does automatically, in six minutes, what can take 6 months manually.
![]() As a result, scientists are gradually equipping themselves with tools capable of helping them distinguish truth from falsehood when it comes to the efficacy of various alternative medicines. The hopes they raise are immense. For this reason alone, they must be assessed with the same rigor as drugs or other biotechnological treatments.
As a result, scientists are gradually equipping themselves with tools capable of helping them distinguish truth from falsehood when it comes to the efficacy of various alternative medicines. The hopes they raise are immense. For this reason alone, they must be assessed with the same rigor as drugs or other biotechnological treatments.
Gregory NinotProfessor of Health, Psychology and Sports Science, University of Montpellier
Visit original version of this article was published on The Conversation.