Will artificial intelligence revolutionize the medical profession?
Coined in the 1950s, the term artificial intelligence (AI) refers to a computer system capable of reasoning, learning, and planning, with behavior reminiscent of intelligent biological systems. Its machine learning is based on programming that is not only determined by code, but also adapts to the data provided to it.
Matthias Brunn, University of Montpellier and William Genieys, Sciences Po – USPC

National Cancer Institute – Unsplash, CC BY
For example, in the formal context of artificial neural networks, mathematical algorithms are used to find, through iteration, the best way to represent the link between several variables. Each neuron represents a fairly simple function, which makes it possible to construct very complex functions in a large network.
Medicine, meanwhile, is an ancient and recognized institution in our societies, as evidenced by the trust placed in healthcare professionals during the COVID-19 pandemic. And we tend to view it as a large ship whose stability cannot be threatened.
However, the reality is quite different. In the coming decades, medicine is likely to be profoundly transformed by AI, a veritable "revolution" according to President Emmanuel Macron. To gauge the scale of these upcoming changes, one need only look at the Health Data Hub, a platform launched by the French government in November 2019 that allows researchers to use data from the national health system to train artificial intelligence models.
Some 10 research projects have already been selected to take advantage of this platform. All of them aim to improve the effectiveness of medicine. For example, "Deepsarc" aims to identify the best treatment regimens for sarcoma, "PIMPON" aims to help prescribers better understand dangerous drug interactions, "Hydro" seeks to predict heart failure episodes in patients with pacemakers, "Oscour" wants to mobilize emergency data to improve health monitoring, and "Deep.Piste" will evaluate the contribution of artificial intelligence to organized breast cancer screening—a major contribution according to a study published last January in Nature and conducted with six radiologists.
While the medical profession has always been able to take advantage of technological innovations (X-rays, MRIs, etc.), it now finds itself facing an unprecedented disruption. Will algorithms take precedence over healthcare professionals? In which disciplines will battles be fought?
A world in constant evolution
According to American sociologists Rue Bûcher and Anselm Strauss, any profession can be defined as a world composed of segments, with different conceptions of their practice and varied identities that transform, maintain themselves, develop, and/or disappear. Various medical disciplines thus find themselves in competition. For example, when it comes to treating serious coronary heart disease, there may be opposition between cardiologists who favor angioplasty and stenting, and cardiac surgeons who prefer open-heart bypass surgery.
Overall, with the support of the state and in competition with other groups such as spiritual healers, the medical profession gained a monopoly on healthcare provision inthe 20thcentury. To achieve this, it relied on a coherent and scientific system aimed at defining, classifying, and diagnosing phenomena of somatic and/or psychological distress. But it was also its ability to self-organize (into disciplines, learned societies, unions, etc.) that gave medicine its authority in health matters.

: Nina Aldin Thune, CC BY-SA
In this context, AI can be seen as a new technical innovation capable of helping doctors, but also of strengthening their power vis-à-vis other disciplines. However, within this highly hierarchical profession, technological choices are made by elites who operate according to a "mandarin" logic, based on a mixture of conservative professional values and rejection of the bureaucratic power of the state. Even if, for each discipline, the decision to use AI depends on a comparative assessment of its benefits and risks, based on past experience.
Psychiatrists are therefore rather skeptical about AI's ability to perform the complex tasks they encounter in their daily work, as psychiatry is generally less keen on technology than other disciplines. Conversely, medical imaging is an area where AI performance is already rendering certain radiologist profiles obsolete. In fact, we are seeing the emergence of a first generation of radiology professors who have built their careers on the use of AI in medical imaging.
High disruptive potential
By going beyond the scope of traditional technical innovations, AI is presenting medical professionals with a veritable revolution. The reasons are primarily technical: in addition to unprecedented speed in performing certain tasks, it enables the development of autonomous learning—as demonstrated by the rapid advances in instant language translation, now available free of charge on the web, with major implications for the job market. But the revolution also comes from the anthropomorphic side of AI...
Artificial neural networks, humanoid robots, and chatbots are examples of this. These digital conversational agents use text- and/or voice-based AI methods to mimic human behavior with evolving dialogue. They are considered a means of providing mental health care in areas where it is scarce, or for people who find it difficult to reveal their feelings to another human being. In short, AI is becoming a social actor in its own right (or an "actant" in Bruno Latour's universe), which increases its disruptive potential.
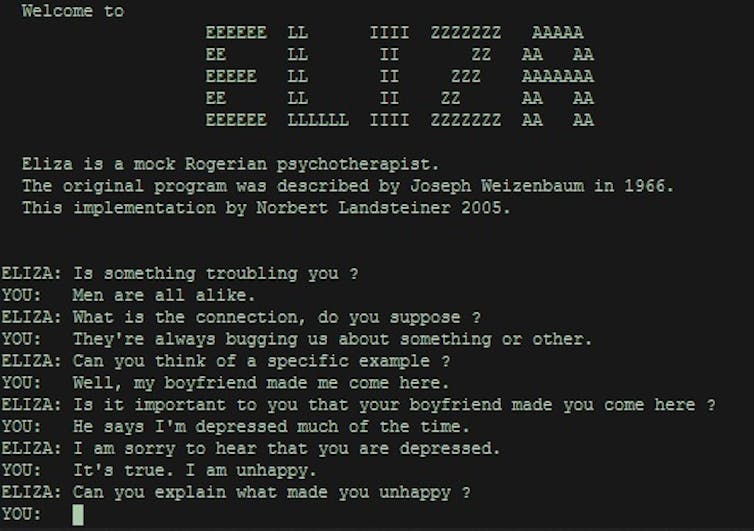
Wikipedia
These two facets of AI go hand in hand and are likely to profoundly transform the world of medicine by disrupting the established order. Radiology, for example, could become a specialty with fewer positions and a more "clinical" than "diagnostic" profile. Conversely, psychiatry, which currently attracts few students, is likely to see its profile strengthened due to its social dimension, which is difficult to replace with AI applications.
In fact, it is precisely by drawing on this dimension and its fundamental virtues (empathy, intimacy of the patient-practitioner relationship, medical confidentiality) that the medical profession as a whole could redefine its profile and scope of action. When it comes to healthcare, various actors outside the medical world have positioned themselves in the treatment of somatic and/or psychological distress through AI: this is particularly the case for
GAFAM companies such as Google, which funds research into AI in healthcare, Facebook, which uses AI to detect suicide risk among its users, and Microsoft, which hosts the Health Data Hub in France.
Like a container ship that, despite being accustomed to storms, can be damaged by a surge of rogue waves, the medical profession is facing an unprecedented situation. And even though it has the necessary resources to navigate, the power of the elements may force it to find a new course. Whatever the outcome, the transformation will be profound.![]()
Matthias Brunn, Political Science Researcher at CEPEL/CNRS, University of Montpellier and William Genieys, CNRS Research Director at CEE, Sciences Po, Sciences Po – USPC
This article is republished from The Conversation under a Creative Commons license. Readthe original article.