To combat back pain, moving more is not enough
“Back pain? The best treatment is exercise.”This slogan has been repeated constantly on television and posters for the past two weeks. The French health insurance system has launched its first national campaign to encourage people suffering from lower back pain to take up physical activity.
Gregory Ninot, University of Montpellier
Shutterstock
The aim of this campaign, which runs until December 18, is to combat the misconception that staying in bed is the best way to recover from a back sprain. Moving around more is certainly beneficial, but is it really that simple?
Back pain affects about 1 in 10 peopleThis persistent pain in the lumbar vertebrae, located just above the coccyx, is called benign or nonspecific low back pain. It causes limited movement, increased sedentary behavior, recurring negative thoughts, emotional difficulties, and repeated absences from work, as established by a study published in 2010.
Some people feel helpless, with nearly 60% of those suffering from low back pain thinking that I would not be able to recoverThey undergo multiple treatments and care without any lasting benefit. And the costs of care for the health insurance system are skyrocketing. A French study of a cohort of people receiving general medical care showed that low back pain lasted more than a year in 81% of patients, with an average total cost per patient over six months of €715 in 2007.
The amount patients have to pay out of pocket is also increasing, as Medicare only reimburses 35 to 70% of healthcare costs, depending on the case.
Movement is necessary
To treat back pain, movement is necessary, as emphasized by the campaignTaking the stairs instead of the elevator, getting off the subway or tram one stop early, using a bike whenever possible to get around, and swimming are a start. These physical efforts are a pain for a gain, much more effective than rest in overcoming lower back pain.

Rest is a bad habit, acquired during episodic illnesses such as the flu. Thinking that rest will cure lower back pain actually makes it worse. The less people move, the less capable they feel of moving. Physical inactivity makes them more vulnerable to other health problems. Low back pain becomes more complicated and chronic. This process is called the vicious cycle of deconditioning.
On the other hand, the danger would be to go too far, too fast, too hard. Taking pain-masking treatments, exercising excessively, or "putting up with it" (blaming aging, professional overwork, burnout, family constraints, etc.) allows you to forget the pain but does not solve anything.
Move more, but not just any old way
Move more, yes, but not just any old way. Research is increasingly exploring the rich field of non-drug interventions. The French National Authority for Health (HAS),Inserm, and the Academy of Medicine are all taking an interest in this area.
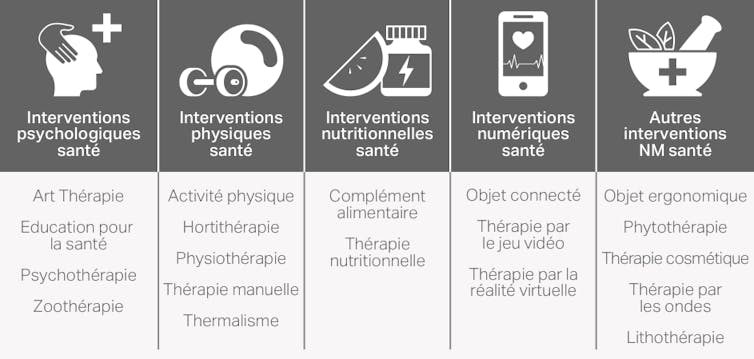
CEPS Platform, Universities of Montpellier
Non-pharmacological interventions (NPIs) specific to low back pain will target muscular aspects (such as strengthening postural muscles), neuromuscular aspects (such as flexibility), neurological aspects (such as pain management), postural (such as workstation), psychological (such as pain desensitization and stress regulation), social (such as work organization), and environmental (such as bedding) aspects.
These NMPs will involve trained professionals, massage therapists, osteopaths, acupuncturists, adapted physical activity (APA) instructors, psychologists, or therapeutic education professionals.
Defining the dose, intensity, and frequency of these NMPs for each person is essential to achieving satisfactory results.
Non-drug interventions have been the subject of clinical studies evaluating their effectiveness in the treatment and prevention of low back pain. These include Pilates, Dru yoga (a form of yoga practiced mainly in Great Britain), tai chi, adapted physical activity programs, osteopathy, chiropractic, acupuncture, spa therapy, the Back School method (an American "back school" founded in 1969), the McKenzie method (originally from New Zealand, created in 1981), and finally therapeutic patient education.

Antonika Chanel/Unsplash
A specific osteopathy program for low back pain
Some studies are particularly interesting. For example, the clinical trial conducted by the team of British doctor and researcher Nefyn Howard Williams evaluated the benefits of an osteopathic method in people suffering from acute and subacute (i.e., low-intensity) spinal pain. The randomized controlled trial included 201 people aged 16 to 65. They had consulted their general practitioner for neck or back pain that had appeared between 2 and 12 weeks earlier.
Comparisons between the group receiving only standard care and the group receiving three to four osteopathic sessions from a trained practitioner were made on three occasions: before the start of the intervention, at the end of the intervention (i.e., two months later), and six months after the intervention. The measurements concerned health status related to spinal pain, quality of life, sensory and emotional dimensions of pain, and the cost-effectiveness of the care received.
The osteopathic sessions were spaced one to two weeks apart, within a maximum time interval of two months. The program included manual techniques and advice on regular physical activity. The results show that, at the end of the two-month osteopathic intervention, there was a decrease in the intensity of spinal pain and an improvement in quality of life compared to the control group.
After six months, quality of life remained higher than in the control group. However, pain levels no longer differed between the two groups. Healthcare costs specific to spinal pain were significantly higher for the group receiving osteopathic treatment (€88 per patient in total).
Psychotherapy tailored to lower back pain
Another study, this time involving psychotherapy. The trial conducted by Swedish researcher Steven Linton's team, published in 2015, evaluates the effectiveness of an intervention carried out with workers and their employers to prevent disabilities caused by back pain. The intervention was compared to standard care for low back pain.
140 people aged 27 to 65 participated in this study, which was conducted in a Swedish health center. They suffered from low back pain and were at high risk of developing chronic musculoskeletal disorders. The researchers recorded each person's days off work due to musculoskeletal disorders, use of healthcare services, perceived health status, and pain intensity. Measurements were taken before and after the intervention, and then six months after the intervention.
Participants in the test group also received a brief psychological intervention based on the principles of cognitive behavioral therapy (CBT). They participated in three face-to-face sessions with a clinical psychologist. Each session lasted between 60 and 90 minutes. The main objective of the intervention was to increase workers' ability to manage the difficulties associated with their experience of pain themselves on a daily basis, particularly in the workplace.
The study shows a twofold reduction in the average number of days off work six months after the intervention (38 days, instead of 17). The difference is statistically significant compared to the control group. The researchers also observed an improvement in perceived health status and a decrease in the use of healthcare services for the test group. The intensity of pain experienced was reduced equally in both groups.
Yoga, a relevant non-pharmacological intervention
Yoga is also one of the relevant non-drug interventions for low back pain. A meta-analysis published in January 2017 reviews all scientific studies on the use of yoga for low back pain and indicates benefits. These yoga programs include physical exercises, breathing exercises, relaxation techniques, and meditation. They promote mindfulness and strengthen the connection between body and mind.
Who should you turn to for help with back pain? The role of the general practitioner and/or specialist is to identify the source of the pain, its severity, and its progression. They can then recommend the most appropriate non-drug treatment for the patient's low back pain—or even several options. This may be in addition to pain medication. This choice is made based on the best balance between benefits and risks, taking into account scientific data, the doctor's experience, the patient's preferences, and the feasibility of the treatment.
![]() General practitioners and specialists are becoming increasingly familiar with NMIs and the local network of professionals who run them. Some health insurance companies are starting to reimburse certain types of exercise. To combat back pain, you need to move more, but above all, move better.
General practitioners and specialists are becoming increasingly familiar with NMIs and the local network of professionals who run them. Some health insurance companies are starting to reimburse certain types of exercise. To combat back pain, you need to move more, but above all, move better.
Gregory NinotProfessor of Health, Psychology, and Sports Science, University of Montpellier
The original version of this article was published on The Conversation.